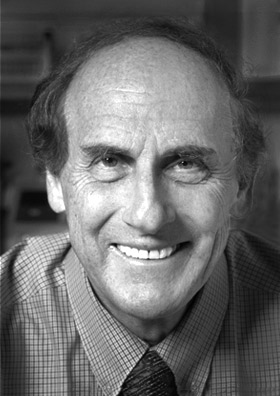
Part XXIII: Ralph M. Steinman, 2011 Prize in Physiology or Medicine
Joseph Luna
A macrophage is on the hunt. Crawling and sniffing its way across a petri dish, this “big eater” lunges forward, its rolling membranes like tank treads, toward a colony of bacteria. A pall descends on the prokaryotes, and soon a membrane washes over them like a toxic blanket. The engulfed bacteria, momentarily stunned, find themselves in the belly of the macrophage and attempt to regain their bearings. They never see the army of lysosomes marching toward them, with acid knives drawn and thirsty.
Zanvil Cohn looked up from his microscope and snapped a photo of the battle below. This phenomenon of cells eating cells, or phagocytosis, was well known immunological territory. But armed with time-lapse microscopy, Cohn could record how the macrophage moved and ate in startling detail; with James Hirsch, Cohn discovered that lysosomes swooped in to digest bacteria when engulfed. Cohn and Hirsch ran a joint lab at the then recently renamed Rockefeller University that was an epicenter of macrophage research in the 1960s. Housed in the Southern Laboratory (now known as Bronk) and under the guidance of the eminent René Dubos, Cohn and Hirsch made landmark discoveries on how these cells defended against microbes, using the latest techniques to finally begin answering questions as old as immunology itself.
Eighty years earlier, a Russian zoologist named Ilya Metchnikoff witnessed the first macrophage chomping on microbes, circa 1882. Such a startling discovery led him to propose that an immune system, at the cellular level, was composed of cells like macrophages on constant patrol for viruses and bacteria. It was an innate and uncompromising system. Yet, there was another equally compelling school of thought, championed by German immunologist Paul Ehrlich, of adaptive immunity, an ever-changing system that could recognize a foreign threat, and remember to counter that specific foreign threat in the future, through the action of what Ehrlich called antibodies. There was never too long of a debate as to which side was right; it was clear that they both were. But missing was the link. How did an adaptive immune response start? How were macrophage foot soldiers connected to cells of the adaptive immune system, the ones who could produce very specific bombs made of antibodies?
These were questions that kept a young medical resident in Boston named Ralph Steinman up all night. Convinced he wanted to go into research, Steinman attended lectures and dived into the immunology literature. He was particularly fascinated with the work of MacFarlane Burnet and his book, The Clonal Selection Theory of Acquired Immunity. Burnet proposed that the immune system was made of a repertoire of cellular clones, each with a unique antigen it sought to destroy. When the antigen showed up, its specific clone expanded rapidly to counter the threat. But missing was how a specific clone knew it was time to expand. One idea was that there might be an accessory cell, one that might instruct adaptive immune cells with parts of the antigen, akin to issuing reports from the front lines with specific coordinates for antibody airstrikes. Among the most promising candidates for such an accessory cell was the macrophage.
Steinman arrived at Rockefeller as a postdoc to work with Cohn in the summer of 1970, set on exploring this idea further. If macrophages could present antigens to adaptive immune cells, it stood to reason that the antigens they encountered weren’t completely destroyed, just taken apart. Except that this didn’t seem to be the case: Cohn’s graduate student, Barbara Ehrenreich, had elegantly documented how macrophages ground down foreign proteins to individual amino acids. Steinman extended this work by feeding macrophages an enzyme called horseradish peroxidase (HRP) that could be used as a tracer both under the microscope and by measuring its enzymatic activity. He found that the macrophages dutifully ate the protein, only to degrade it all the way to single amino acids, just as Ehrenreich had observed. HRP activity followed a similar course and gradually, but completely, disappeared.
So it appeared that macrophages from the mouse peritoneal cavity weren’t able to keep intact antigens around. Steinman decided to look somewhere else. It was known since the 1930s that the spleen was an organ where an immune response could begin, and only in 1966 were researchers in California able to generate an immune response from suspensions of mouse spleen cells. With this in mind, Steinman took mouse spleens, ground them up, and plated the cells onto glass dishes. Adherent cells like macrophages stuck to the glass, as was the standard practice to isolate them. As he peered into the microscope, fully expecting lysosome-rich macrophages prowling about, he saw something quite different: cells with numerous extended processes, like branches of a tree. Being in an expert macrophage lab, Steinman and Cohn were quickly able to document all the strange differences between this new cell, which they named a dendritic cell, and the usual adherent roamers. Dendritic cells had few lysosomes, were poor at engulfing tracers like HRP, and didn’t move around so much as constantly extend and retract their limbs, probing about. These cells were relatively rare (about 1% of spleen cells) and difficult to isolate, but by the mid 1970s the then Cohn-Steinman lab discovered that a single dendritic cell was a hundred times more potent at inducing an immune response. Over the next four decades, the Steinman lab discovered all sorts of functions, mechanisms and potential therapeutic uses for dendritic cells. Like branches on a well-rooted tree, a field was born.
